Aquablation is a surgical treatment for benign prostatic hyperplasia (BPH), which means a non-cancerous enlargement of the prostate gland. The prostate sits below the bladder and surrounds the urine tube (urethra). When it enlarges, it can restrict urine flow and cause lower urinary tract symptoms (LUTS), such as a weak stream, straining, urgency, frequent urination, and waking at night to pass urine.
One of the most common and sensible questions men ask before treatment is:
“How likely am I to have complications?”
This article focuses on real-world safety and complication risk, not promotional claims. It explains:
- What complications can occur
- How often they happen based on published evidence
- What usually happens if a complication develops
- Why real-world outcomes can differ from clinical trials
The aim is to provide clear, practical expectations, particularly relevant to UK practice across both the NHS and the independent sector.
What Is Aquablation, and Why Do Patients Worry About Complications?
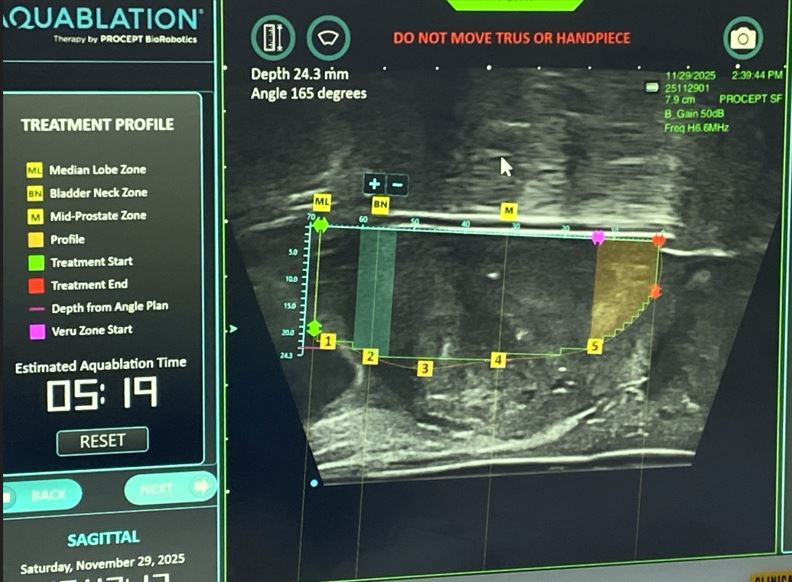
Aquablation uses a robotically controlled, high-pressure water jet to remove prostate tissue that is blocking urine flow. The surgeon plans the treatment using real-time ultrasound imaging, and the robotic system follows this plan with high precision.
Patients commonly worry about complications because:
- The prostate has a rich blood supply
- Surgery is performed through the urethra
- Recovery experiences vary widely
- Much online information comes from hospital or device -led marketing
Understanding realistic risks, rather than idealised outcomes, helps patients make informed decisions and reduces anxiety around recovery.
What Types of Complications Can Happen After Aquablation?
Based on NICE, complications after Aquablation can be grouped into several categories:
- Bleeding, early or delayed
- Infection, most commonly a urinary tract infection (UTI)
- Temporary difficulty passing urine after catheter removal
- Urethral stricture, meaning scar-related narrowing of the urethra
- Urinary incontinence, which means leakage of urine
- Need for further treatment in the future
Most complications are temporary and manageable, but some require additional treatment or short hospital readmission.
How Common Is Bleeding After Aquablation, and How Often Is It Serious?
Mild bleeding
Seeing some blood in the urine (haematuria) is common after all prostate operations. It usually:
- Occurs in the first days or weeks
- Improves gradually with time and good hydration
- Does not require further treatment
Bleeding needing intervention
More significant bleeding may lead to:
- Blood clots blocking urine flow
- A drop in haemoglobin (the blood count)
- Readmission to hospital
Real-world published data suggests:
- Around 2–4% of men require a blood transfusion
- Risk is higher in very large prostates
- Rates tend to fall as surgical teams gain experience
Why bleeding happens?
- Larger prostates leave a greater raw surface area
- The prostate contains many blood vessels
- Technique and experience influence bleeding control
If significant bleeding occurs, treatment may include:
- Continuous bladder irrigation through a catheter
- Temporary catheter traction
- Endoscopic clot removal and cauterisation
- Blood transfusion if necessary
How Likely Is Infection After Aquablation Surgery?
A urinary tract infection (UTI) is one of the most common short-term complications.
Evidence from published studies shows:
- 7–12% of men develop a UTI, most often within the first month
Why infections occur
- Temporary catheter use
- Inflammation of the bladder and prostate
- Incomplete bladder emptying during early recovery
Most UTIs are treated with antibiotics based on urine test results and settle without long-term problems.
How Common Are Urethral Strictures After Aquablation?
A urethral stricture is a narrowing of the urethra caused by scar tissue. It can result in:
- Weak urine stream
- Straining to pass urine
- Recurrent urine infections
Published data indicate:
- Urethral strictures requiring treatment occur in around 2–3% of patients
Strictures usually develop months after surgery, not immediately.
Treatment may involve:
- Camera inspection (cystoscopy)
- Stretching or cutting the scar tissue
- Rarely, more complex reconstruction for recurrent strictures
Can Aquablation Cause Long-Term Urinary Incontinence?
Urinary incontinence means involuntary leakage of urine.
Temporary urgency or mild leakage is common early on and usually improves as healing occurs.
Persistent long-term incontinence is uncommon:
- Reported at around 2% in longer-term follow-up studies
Why long-term leakage may occur
- Temporary irritation of the urinary sphincter
- Pre-existing bladder overactivity
- Nerve sensitivity rather than permanent muscle damage
How Often Do Men Need Further Treatment After Aquablation?
Needing another procedure for prostate symptoms is called retreatment.
Real-world follow-up data suggests:
- Approximately 4% of men require further treatment within 4 years
Reasons include:
- Residual prostate tissue
- Regrowth of tissue over time
- Scar-related narrowing at the bladder neck
This rate is broadly comparable with other surgical treatments for BPH.
Why Do Complication Rates Differ Between Clinical Trials and Real-World Practice?
This difference is important when interpreting online statistics.
Clinical trials:
- Carefully selected patients
- Exclusion of higher-risk cases
- Performed in specialist centres
- Strict monitoring and follow-up
Real-world practice:
- Broader patient population
- Larger prostates
- More medical complexity
- Variation in surgeon experience
In UK practice, this distinction is particularly relevant, as patients treated across both the NHS and the independent sector often differ from those enrolled in tightly controlled international trials. As a result, trial data may underestimate everyday complication risk.
What Are the Real-World Aquablation Complication Rates Patients Should Expect?
Based on currently available evidence, realistic ranges are:
- Urinary tract infection: 7–12%
- Bleeding requiring transfusion: 2–4%
- Urethral stricture: approximately 2–3%
- Persistent urinary incontinence: around 2%
- Further treatment within 4 years: around 4%
These figures are consistent with outcomes reported across mixed healthcare systems and align with UK patient expectations for transparency around surgical risk.
Where Do These Aquablation Complication Figures Come From?
The complication rates quoted above are derived from published peer-reviewed medical studies, real-world cohort analyses, and independent evidence summaries. They are based on outcomes reported in everyday clinical practice rather than manufacturer brochures, promotional hospital material, or single-centre marketing reports.
This approach better reflects realistic patient experience, including variation related to prostate size, surgical technique, and healthcare setting.
Why this matters:
Real-world data provide a more accurate picture of what patients are likely to experience outside highly controlled trial environments.
What Happens If a Complication Occurs After Aquablation?
Most complications are:
- Identified early
- Treated effectively
- Temporary
Management may include:
- Catheter reinsertion for temporary urine retention
- Antibiotics for infection
- Endoscopic procedures for bleeding or scarring
Understanding what usually happens if something goes wrong often reassures patients more than percentages alone.
Frequently Asked Questions About Aquablation Complications
Is Aquablation safer than TURP?
Safety profiles differ. Aquablation may reduce some sexual side effects but has a distinct bleeding risk profile, particularly in larger prostates.
Does prostate size increase complication risk?
Yes. Larger prostates are associated with higher bleeding risk and slightly higher retreatment rates.
How long do Aquablation side effects last?
Most urinary symptoms improve over several weeks. Mild bleeding may last longer. Long-term problems are uncommon.
Are complications greater outside specialist centres?
Real-world data suggests that complication rates may be higher early in a center’s experience, particularly before techniques are standardised.
Why Large Real-World Aquablation Safety Registries Are Still Needed
Much of the available data comes from:
- Clinical trials
- Single-centre reports
- Industry-linked studies
What remains limited are:
- Large, independent, multi-centre registries
- Standardised definitions of complications
- Long-term continence and stricture tracking
It is especially important in the UK, where wider adoption across both NHS and independent providers makes comprehensive, non-promotional outcome tracking essential.