What Is a Radical Prostatectomy and When Is It Used for Prostate Cancer?
A radical prostatectomy is an operation to remove the entire prostate gland, often used to treat localised prostate cancer. This surgery may be:
- Open surgery (through a single cut in the lower abdomen)
- Laparoscopic (keyhole) surgery
- Or more commonly now, robot-assisted surgery
The main goals of radical prostatectomy are
- Removing all the cancer
- Preserving bladder control (continence)
- Protecting erections (sexual function)
- Avoiding complications
Why Does the Surgeon’s Learning Curve Matter in Prostate Cancer Surgery?
Surgeons improve with practice. The learning curve is the number of operations it takes for a surgeon to become skilled and consistently get good results.
In the early stages of learning, a surgeon may:
- Take longer to complete the operation
- Be more likely to leave positive surgical margins (where some cancer is left behind)
- Be less confident in preserving the nerves that control erections
- Cause more blood loss or surgical complications
Surgeons who are past the learning phase (usually after around 100 operations) tend to
- Perform surgery faster
- Get better cancer control
- Reduce side effects and complications
- Preserve continence and potency more often
What Are Pentafecta Outcomes After Prostate Removal Surgery?
Doctors often measure success using the “pentafecta”—five ”key — five key outcomes that matter most after prostate cancer surgery:
- Cancer control—no rise in PSA after surgery (no signs of cancer returning)
- Urinary continence—not needing pads or experiencing urine leakage
- Sexual potency—being able to get erections after surgery
- Negative surgical margins—no cancer cells at the edges of the removed prostate
- No complications—avoiding serious problems during or after surgery
These outcomes give a complete picture of how well the surgery went.
What Did the 2025 Study Reveal About Surgeon Experience and Prostate Cancer Outcomes?
A large systematic review and meta-analysis published in BMC Urology (July 2025) looked at:
- 16 studies involving 21,851 patients
- Comparing outcomes between surgeons early in training vs experienced surgeons
- Outcomes reviewed: cancer control, bladder control, erections, complications, bleeding, and more
Here’s what they found:
Does Surgeon Experience Influence Cancer Recurrence After Prostatectomy?
- The biochemical recurrence (return of cancer, measured by rising PSA) was similar in both groups.
- However, there was a slight trend towards better cancer control among in experienced surgeons.
- So while not statistically significant, it still favoured experience.
What this means for patients: An experienced surgeon may have a slightly better chance of removing all the cancer.
Are Urinary Continence Rates Better with Experienced Prostate Surgeons?
- Patients operated on by experienced surgeons were more likely to regain full bladder control.
- The difference was small but consistent across studies.
Why? Preserving the urinary sphincter and avoiding damage to surrounding tissues improves with surgical skill.
Do Positive Surgical Margins Occur More with Inexperienced Surgeons?
Yes—clearly.
- The risk of positive margins was 61% higher in surgeons early in their learning curve.
- Positive margins mean some cancer may be left behind, raising the chance of needing further treatment.
This was the strongest and most consistent difference between early and experienced surgeons.
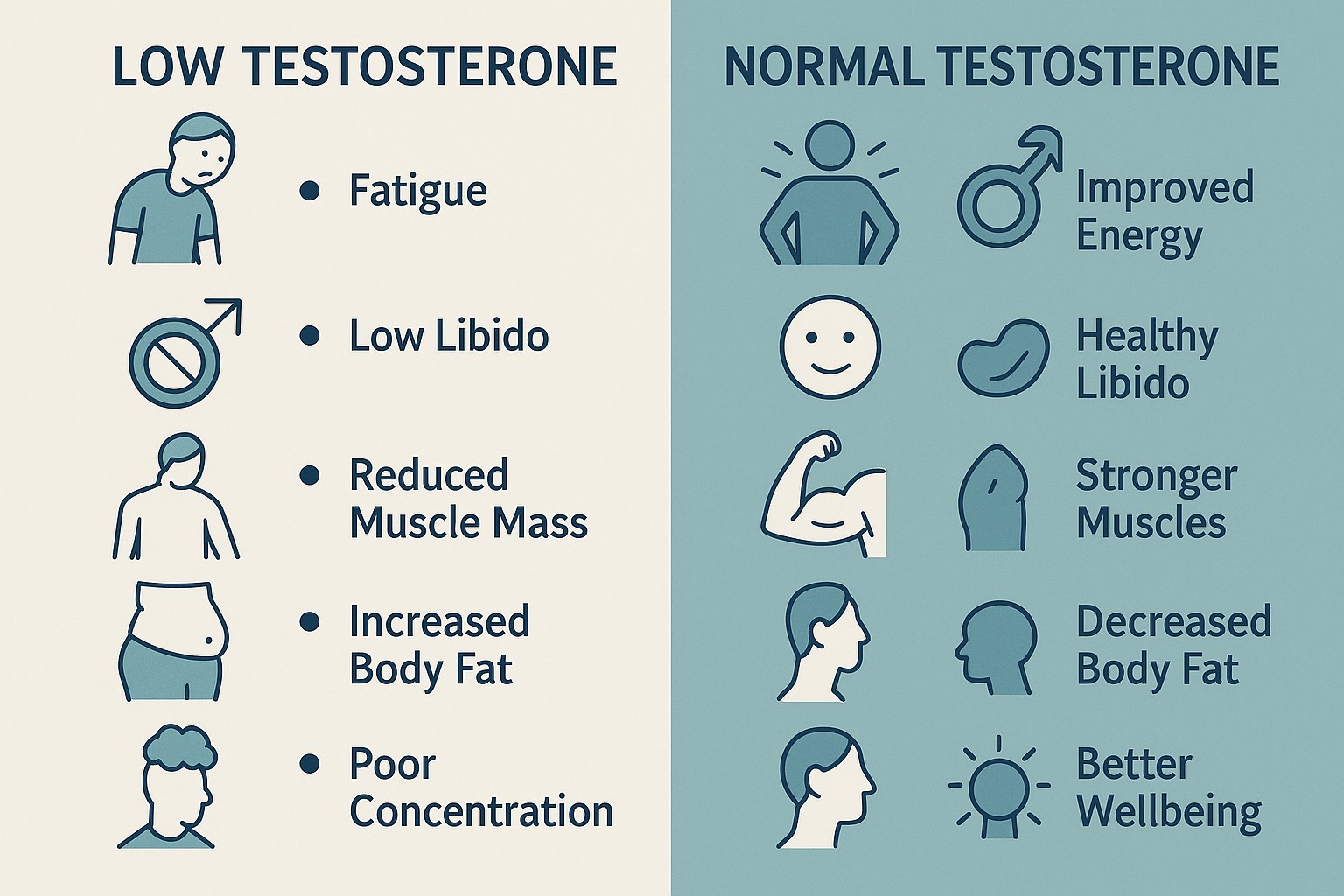
Can Surgeon Experience Improve Erectile Function After Prostate Cancer Surgery?
Yes. The study found that:
- Potency outcomes (return of erections) were better in men treated by experienced surgeons.
- This is because preserving the neurovascular bundles (the nerves for erections) is technically challenging.
Nerve-sparing surgery is one of the most difficult parts of prostatectomy and improves with experience.
How Does Surgeon Experience Affect Complications, Blood Loss, and Surgery Time?
Surgeons with more experience had:
- Shorter operations
- Less blood loss
- Fewer complications (like infections or needing a return to theatre)
These benefits lead to safer surgery and faster recovery.
How Many Surgeries Are Needed for a Surgeon to Become Skilled in Prostatectomy?
The analysis showed that after around 100 operations, most surgeons:
- Had lower complication rates
- Achieved better functional outcomes
- We're more likely to deliver pentafecta results
This number is often used as a benchmark for reaching a consistent and reliable level of skill.
What Should Patients Ask Their Surgeon Before Prostate Cancer Surgery?
Before having a radical prostatectomy, it’s reasonable to ask questions like:
- How many radical prostatectomies have you performed?
- Do you perform nerve-sparing surgery routinely?
- What are your typical outcomes for:
- Bladder control?
- Sexual function?
- Positive margin rates?
- Will a more experienced surgeon be supervising or involved?
Asking these questions can help you make a confident and informed decision.
Why Choosing a High-Volume Centre for Prostate Cancer Surgery Matters
Research consistently shows that:
- Hospitals and surgeons who do more prostate surgeries have better results
- They are more likely to:
- Avoid complications
- Preserve continence and potency
- Completely remove the cancer
- These centres also tend to have better training, support, and equipment
Even if a trainee is involved, they are often closely supervised in these settings.
Summary: Surgeon Experience Strongly Influences Prostate Cancer Surgery Outcomes
If you’re having prostate cancer surgery, the experience of your surgeon matters. According to current research:
- Cancer removal is more complete with experienced hands
- Bladder control and sexual function recover more reliably
- Surgery is safer and shorter with less blood loss and fewer complications
- Outcomes improve significantly after 100 operations
Choosing a surgeon or centre with high case volumes can make a real difference in your results and recovery.