Men often ask whether their weight affects prostate cancer once they already have the diagnosis. The simple answer is yes—weight after diagnosis can influence cancer recurrence, long-term outcomes, general health, and even survival.
This article explains, in clear language, what the evidence shows about weight gain, weight loss, and prostate cancer outcomes—and how men can protect their health.
Why Does My Weight Matter After a Prostate Cancer Diagnosis?
Your weight after diagnosis affects more than just how you feel physically. It influences:
- Cancer recurrence (the cancer coming back)
- Cancer progression (how the tumour behaves over time)
- Overall health and survival
- Heart health, especially if you are on hormone therapy
- Muscle strength, energy levels and recovery
Fat tissue is not just “extra weight.”. It behaves like an active organ that produces hormones and inflammatory substances that can impact cancer cells.
Does gaining weight after diagnosis increase my risk of cancer returning?
Yes. Several studies show that weight gain after prostate cancer diagnosis—especially around the time of prostatectomy— is linked with a higher risk of recurrence.
A landmark study found that men who gained as little as 2–5 kg in the period around surgery had almost twice the risk of recurrence compared with men whose weight stayed stable.
Why does such an event happen?
- Extra fat tissue increases insulin and insulin-like growth factors, which act as growth signals for cells.
- It increases inflammation, which can encourage cancer activity.
- It may change hormone balance in a way that promotes cancer growth
These effects make weight gain after treatment a vital factor for men to understand and manage.
What Does the Latest Research Show About Weight Change After Diagnosis?
A major 2025 meta-analysis (a study that combines data from many other studies to produce a more reliable answer) included over 12,000 men and examined how weight change affects outcomes.
Here are the key findings, explained:
Weight Gain After Diagnosis
Weight gain after diagnosis was linked with:
- 23% higher risk of dying from any cause
(This means that for every 100 men who would be expected to die over a specific period, an additional 23 men died in the group who gained weight.) - 64% higher risk of dying from prostate cancer specifically
(This is a significant increase — it means prostate cancer was more likely to be the cause of death in men who gained weight.)
Weight Loss After Diagnosis
Weight loss after diagnosis was linked with:
- 54% higher risk of dying from any cause
Weight loss does not mean intentional; healthy weight loss is harmful.
Instead, this finding likely reflects:
- Unintentional weight loss
- Poor appetite or poor intake, especially during treatment
- Loss of muscle, known medically as sarcopenia (low muscle mass, which weakens the body)
In other words, the problem is not healthy weight management — it is sudden or unplanned weight loss, which can be a sign of underlying illness.
Understanding the “U-Shaped Effect”
The study shows a U-shaped effect:
- Too much weight gain → worse outcomes
- Too much weight loss → also worse outcomes
Staying in the middle of the “U”—maintaining a steady, healthy weight—is linked with the best outcomes.
The U-shaped data demonstrates why weight stability is essential after diagnosis: it avoids both extremes that can harm long-term health.
Is Losing Weight Good or Bad After Treatment?
It depends on how and why weight loss occurs.
Intentional Weight Loss — Usually Positive
If you are overweight or obese, gradual, planned weight loss is usually beneficial.
This type of weight loss involves:
- Health-focused diet changes
- Increased physical activity
- Preserving muscle through strength exercise
Benefits include:
- Reduced visceral fat (fat stored around the organs)
- improved insulin sensitivity
- healthier hormone balance
- reduced inflammation
- improved heart health
These changes create a biological environment that is less supportive of cancer growth.
Unintentional or Rapid Weight Loss — Often Concerning
Unplanned weight loss usually means:
- poor nutrition
- reduced appetite
- muscle loss
- underlying illness or inflammation
- depression or stress
This type of weight loss weakens the body and increases the risk of complications.
The meta-analysis shows higher overall mortality in men who lost weight, not because losing fat is harmful, but because losing weight without trying is a warning sign.
How Does Obesity Affect Prostate Cancer Treatments?
Surgery (including robotic prostatectomy)
Obesity can affect:
- operative time
- technical difficulty
- access to structures around the prostate
- continence recovery
- wound healing
Some studies show slightly higher rates of positive surgical margins (cancer cells at the edge), although results vary.
Radiotherapy
Men with obesity may experience:
- More movement of pelvic organs
- Challenges in delivering precise radiation doses
- Slightly worse biochemical control in some studies
Being obese does not mean radiotherapy is unsafe — simply that weight management helps optimise treatment accuracy.
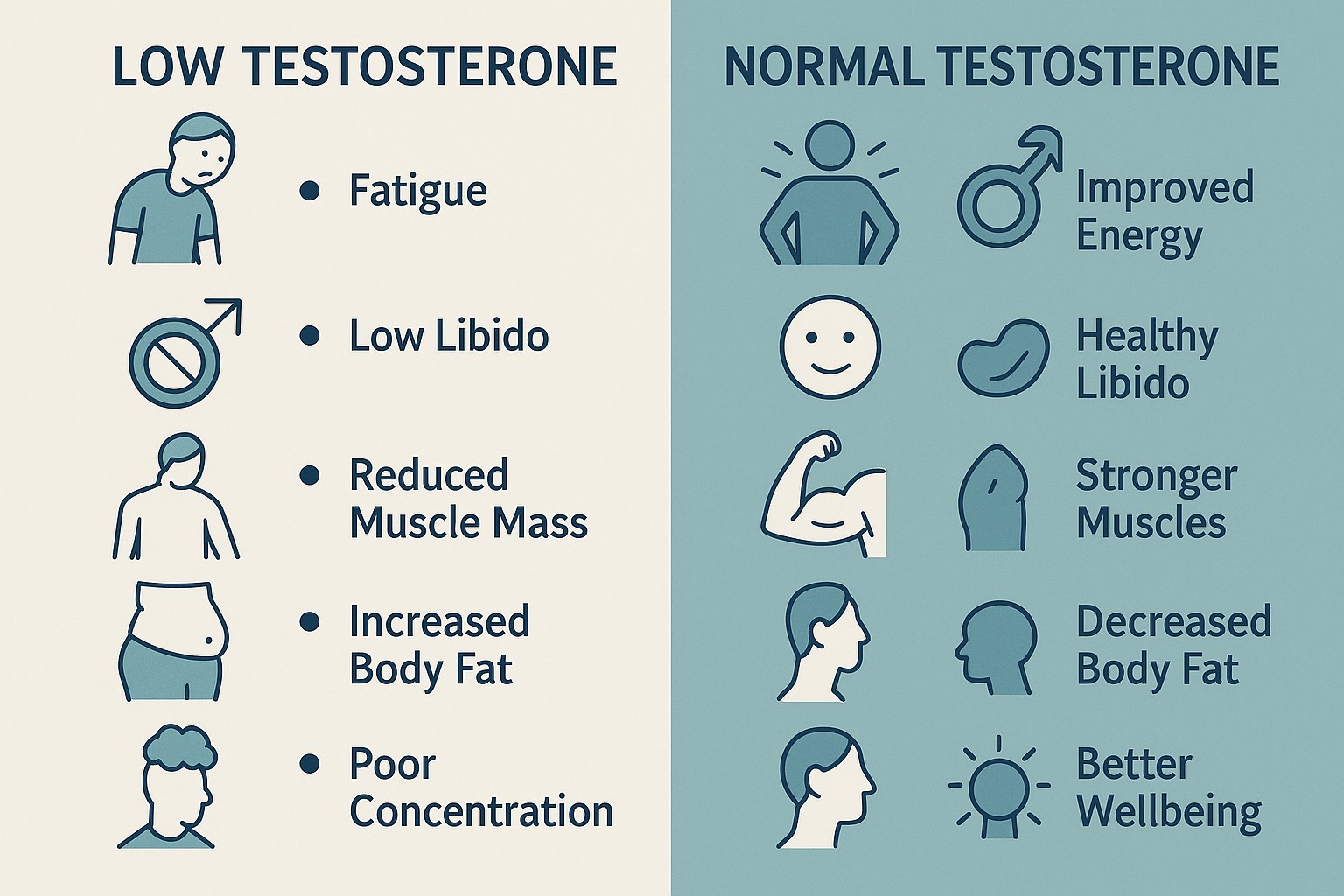
Therapy (ADT)
Androgen Deprivation Therapy (ADT)—a treatment that lowers testosterone—is widely used for prostate cancer.
ADT commonly causes:
- Increased body fat
- Reduced muscle
- Metabolic syndrome (a combination of high blood pressure, high blood sugar, abnormal cholesterol and increased waist size)
- increased heart risk
Maintaining a stable weight, preserving muscle, and staying active significantly reduces these complications.
What Weight Should I Aim For After Diagnosis?
A beneficial general target is:
- BMI between 20 and 25
- Waist circumference below 94 cm
- Avoiding more than 3–5% weight gain after treatment
- If overweight, aiming for slow weight loss (0.25–0.5 kg per week)
- Maintaining or increasing muscle mass through strength exercise
These targets reduce inflammation, improve hormone balance, and protect long-term health.
How Can I Manage My Weight Safely During and After Treatment?
Practical Nutrition Steps
- Eat lean protein to help maintain muscle.
- Base meals on vegetables, whole grains, legumes and healthy fats.
- Limit processed foods and sugars.
- Reduce excess calories slowly and steadily.
- Keep alcohol within recommended limits.
Practical Exercise Steps
- Aim for 150 minutes of moderate exercise each week.
- Include strength training twice weekly.
- Walking, cycling and swimming help reduce body fat
- Strength exercises maintain muscle and improve recovery after surgery and ADT.
- Start gently and build gradually, especially after prostatectomy.
Monitoring Your Progress
Track:
- Weight.
- Waist size.
- Strength (ability to climb stairs, lift items).
- Energy and sleep.
- blood pressure, cholesterol and glucose (especially on ADT)
A holistic approach paints a clearer picture than weight alone.
Key Facts Every Man Should Remember
- Weight after diagnosis matters as much as weight before diagnosis.
- Gaining weight increases the risk of recurrence and prostate cancer death.
- Losing weight unintentionally is also harmful because it often leads to muscle loss or illness.
- The safest approach is maintaining a stable, healthy weight.
- Planned, gradual weight loss in overweight men is beneficial.
- Preserving muscle is as important as reducing fat.
- Weight management is part of cancer survivorship, not just general health.
FAQs About Weight and Prostate Cancer
Does belly fat increase prostate cancer risk after diagnosis?
Yes. Belly fat is visceral fat, which produces hormones and inflammatory chemicals. These can promote aggressive cancer behaviours.
Is it safe to lose weight during hormone therapy?
Yes—if the weight loss is planned, gradual, and includes muscle-preserving exercises.
Why is unintentional weight loss harmful?
It often means muscle loss, poor nutrition, or underlying illness.
Can exercise reduce my risk of recurrence?
Regular exercise improves insulin levels, reduces inflammation and supports overall health — all factors linked with better prostate cancer outcomes.
What weight gain is too much?
More than 3–5% of your body weight is linked with worse outcomes.
Does obesity affect PSA levels?
Yes. Obesity can dilute PSA levels in the bloodstream, making them appear lower than they truly are. It may delay diagnosis or mask progression.
Is weight management part of prostate cancer survivorship?
Absolutely. It reduces the risk of recurrence, improves treatment tolerance, and protects heart health.