If you’ve been told you need a robotic prostatectomy and you have a body-mass index (BMI) in the obese range, you might be wondering how your weight will affect your surgery and recovery. This article explains the latest evidence — in plain terms — and what you can do beforehand to improve outcomes
What the Research Shows: Key Facts About Obesity and Robotic Surgery Outcomes
A major BMC Urology 2024 meta-analysis reviewed data from over 12,000 patients who underwent robotic prostatectomy. It found clear trends between BMI and surgical outcomes
Outcome Obese Patients Non-Obese Patients Difference
Operation TimeLonger (by 18 minutes) Shorter ⬆ More time needed
Hospital Stay 0.18 days longer Shorter stay⬆︎ Slightly longer
Blood Loss More bleeding Less bleeding⬆︎ Technically more difficult
Complication Rate 1.6× higher Lower⬆︎ Significantly higher
Major Complications 30% higher Lower ⬆︎ Increased surgical risk
Incontinence at 1 Year 17% more likely Less incontinence⬆︎ More pad use
Erectile Dysfunction 8% more likely Better recovery⬆︎ Slight reduction in potency
Positive Surgical Margins 20% more likely Lower PSM⬆︎ Higher risk of recurrence
In short: robotic technology helps level the field, but obesity still increases recovery time and complication risk.
What is robot-assisted radical prostatectomy?
Robot-assisted radical prostatectomy (RARP) is a high-precision, minimally invasive procedure to remove the prostate gland when treating localised prostate cancer.
It uses robotic arms controlled by the surgeon from a console, offering:
- Smaller cuts
- Less bleeding
- Faster recovery
- Better chance of preserving erections and continence
Why Robotic Surgery Still Offers Benefits — Even for Obese Patients
Compared with open surgery, robotic systems provide:
- 3-D magnified vision, improving accuracy despite fatty tissue.
- Fine wristed instruments, allowing delicate dissection in tight pelvic spaces.
- Smaller incisions, meaning lower wound-infection rates and faster healing.
- Better preservation of nerves controlling urinary and sexual function.
Several studies confirm that even in obese patients, robotic surgery reduces hospital stay and blood loss compared to traditional methods.
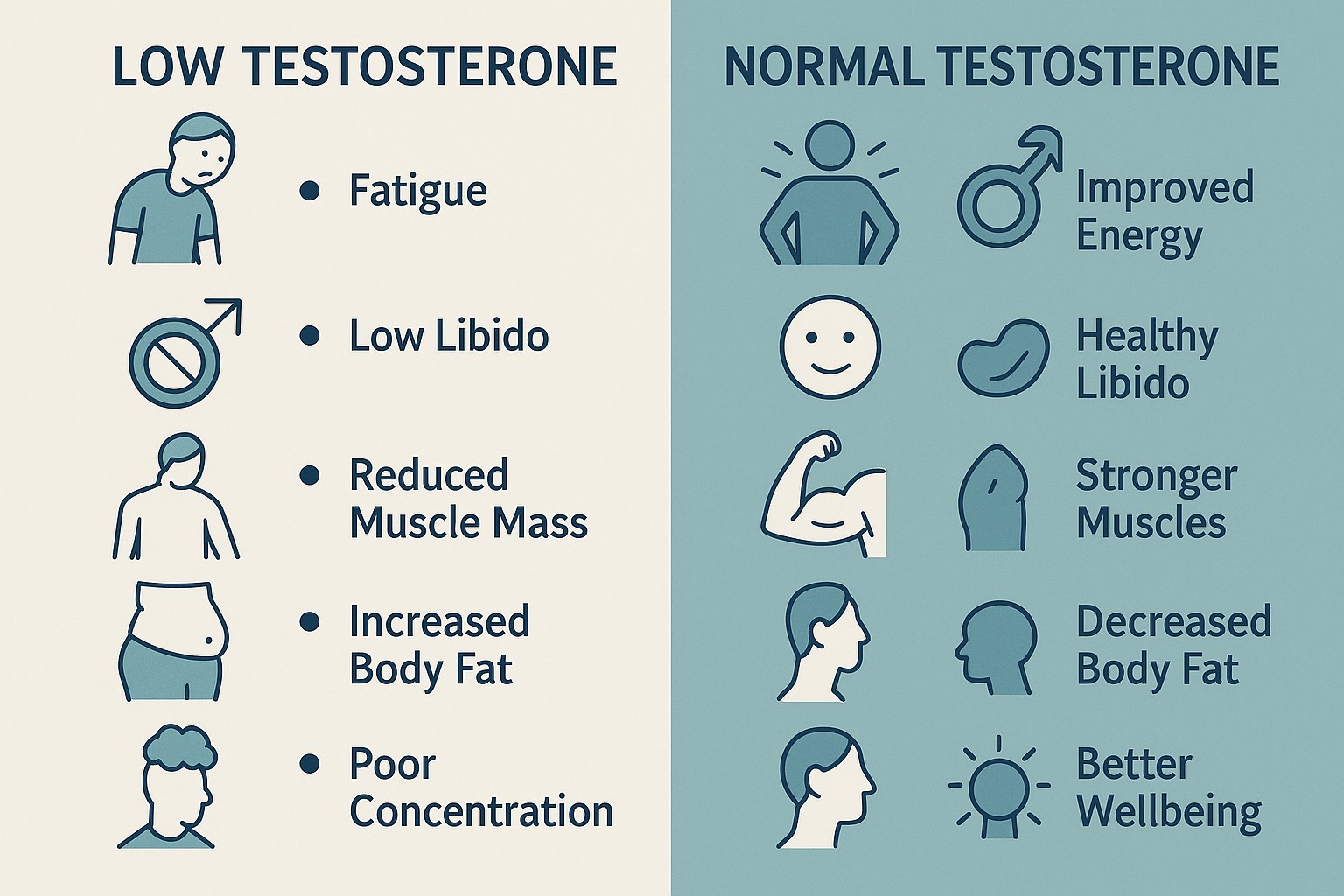
Why Is Obesity a Concern in Prostate Cancer Surgery?
Obesity is defined as a BMI of 30 or above. It affects about 25% of UK men, according to theNHS.
In prostate cancer, obesity can:
- Make surgery more complex
- Delay healing
- Increase the risk of complications
- Reduce cancer control
This review looked at how obesity impacts outcomes specifically after robotic prostatectomy.
How Does Obesity Affect the Surgery and Recovery?
- Operating Time: On average, 18 minutes longer in obese men.
- Hospital Stay: Around 4 hours longer.
- Blood Loss: Increased by about 50 ml.
These differences are linked to:
- More abdominal fat around the prostate
- Reduced visibility and space during surgery
- Higher blood supply to fatty tissues
Are There More Complications in Obese Patients?
Yes. The review showed a clear rise in complication rates:
- Overall complications were 60% higher
- Major complications were 30% higher
- Minor complications (e.g. infections) were also more common
Does Obesity Affect Continence and Erections?
Continence:
- Obese men were 17% more likely to be incontinent at 1 year.
- Reasons include:
- Weaker pelvic floor support
- Difficulties sparing nerves and muscles during surgery
Erectile Function:
- 8% more likely to experience erectile dysfunction
- More fat around the neurovascular bundles makes it harder to preserve these critical structures
Does Obesity Impact Cancer Outcomes?
Positive Surgical Margins (PSM):
- Risk was 20% higher in obese patients.
- This means some cancer cells were left at the edge of the prostate, increasing the risk of recurrence.
Will Losing Weight Before Surgery Help?
Yes — the study authors suggest that weight loss before surgery can:
- Improve visibility and ease of surgery
- Reduce operation time and blood loss
- Lower risk of complications
- Improve recovery of continence and potency
- Possibly reduce the chance of cancer recurrence
Even losing 5–10% of body weight can lead to noticeable benefits.
Robotic Prostate Surgery in the UK: What Patients Should Know
If you are obese and have been diagnosed with prostate cancer, you can still undergo robotic prostate surgery in the UK.
In the private sector:
- Many centres across the UK offer robotic prostatectomy using the da Vinci system.
- Prehabilitationg diet advice, weight loss support, and physical fitness — may be available to help improve your outcome.
If your BMI is over 30, your urologist may still recommend surgery but with extra precautions to reduce risks and support your recovery.
Frequently Asked Questions (FAQs)
What BMI is considered too high for robotic prostate surgery?
There is no absolute cut-off. However, a BMI > 40 kg/m² (morbid obesity) significantly increases risk, so your surgeon will evaluate whether weight loss first would be safer.
How long will I stay in hospital?
Most patients are discharged within 24–48 hours. Some obese men may need an extra day for monitoring, especially if sleep apnoea or wound issues are present.
Can weight loss before surgery improve outcomes?
Yes. Even modest weight loss (5–10 %) can reduce complications, shorten hospital stay, and improve continence recovery.
What if I can’t lose weight before surgery?
Your surgeon can still perform a robotic prostatectomy safely, but you know your risk of complications is higher.
Why This Information Matters for You
Understanding how obesity affects your surgery helps you take control before the operation. By addressing weight, fitness, and general health, you’re not just improving surgical safety — you’re also:
- Enhancing urinary control recovery.
- Supporting erectile function recovery.
- Reducing infection and wound complications.
- Shortening your return-to-normal time.
Can Obese Men Still Benefit from Robotic Prostate Cancer Surgery?
Absolutely. Robotic surgery remains a safe and effective treatment for prostate cancer in obese men. However, the risks are slightly higher, and personalised counselling is essential.
Weight loss, even before surgery, can make a meaningful difference to outcomes, both in terms of safety and cancer control.
For men with obesity, a robotic approach in expert hands—paired with thoughtful preparation—remains a valuable option in the fight against prostate cancer.
References
- BMC Urology (2024) – Perioperative, functional, and oncologic outcomes in obese patients undergoing Da Vinci robot-assisted radical prostatectomy. Link
- NHS UK – Obesity overview
- Prostate Cancer UK – Living well after prostate cancer surgery